Envisioning a coordinated care, out of hospital, virtual observation pathway
Goals of Project
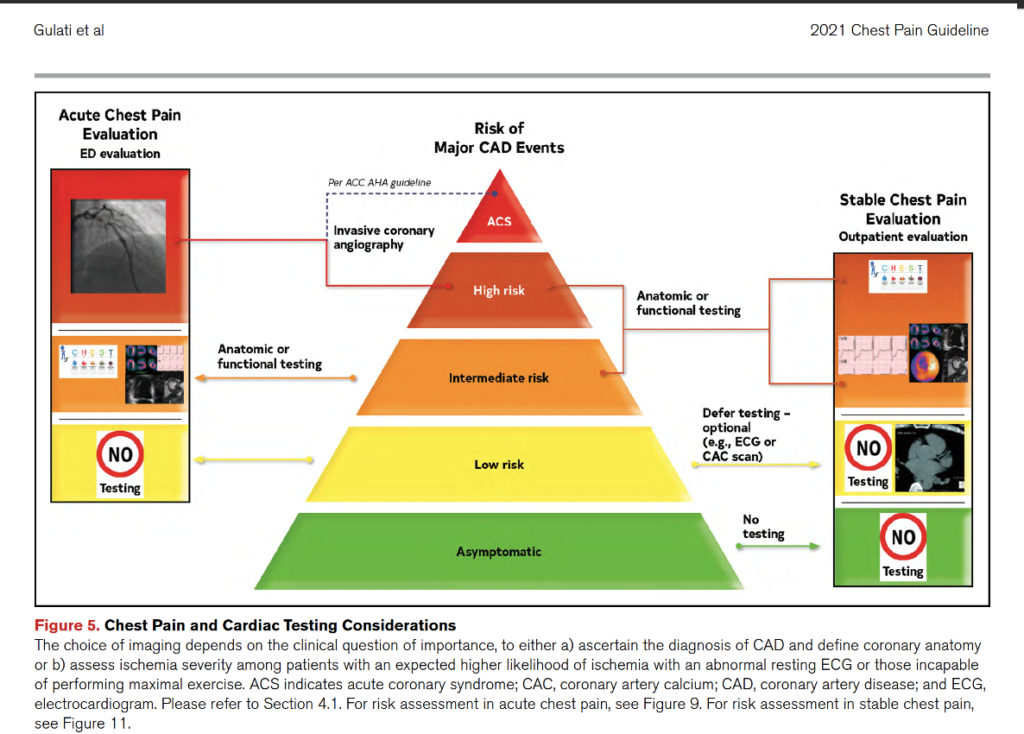
- Over the last 3-5 years, we have developed more comprehensive risk stratification of chest pain concerning for ACS in the ED with implementation of the HEART score and pathway specific flow for patients with low, intermediate, and high risk scores
- The utilization of 3 hour Delta Trop is standard for the patient with a <= 3 HEART and no known disease
- In September 2018, we opened the ED CDU. In the ED CDU we also began to further stratify intermediate risk (and refine our comfort around low risk). Intermediate risk followed a CCTA strategy that also evolved over time and included ASCVD Risk Calculation and utilization of statins and asa and targeted cardiology consult, decreasing consult utilization and downstream testing.
- The model was successful with daily use of CCTA, increased ED D/C, low rates of adverse outcomes outcomes, and identification of disease, short LOS, low variability
- Chest pain work up across hospital/institution with high variability in diagnostic approach and long LOS
- ED CDU currently closed with Covid and volume
Review of Current ED/ED CDU Chest Pain Pathway
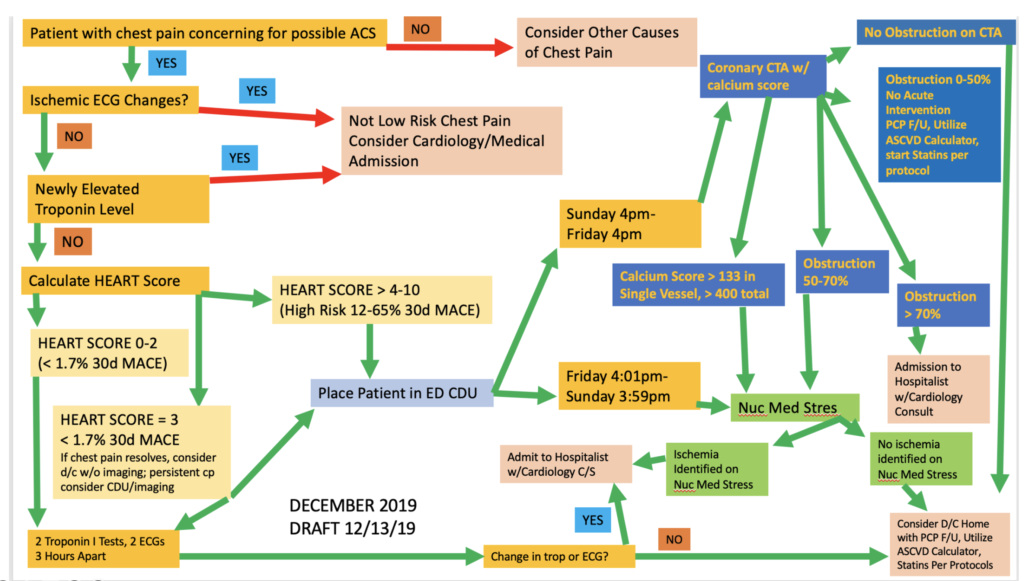
Low Risk already Integrated into Pathway with Early Discharge (“delta trop”) and no diagnostic testing. The HEART score is utilized for this approach.
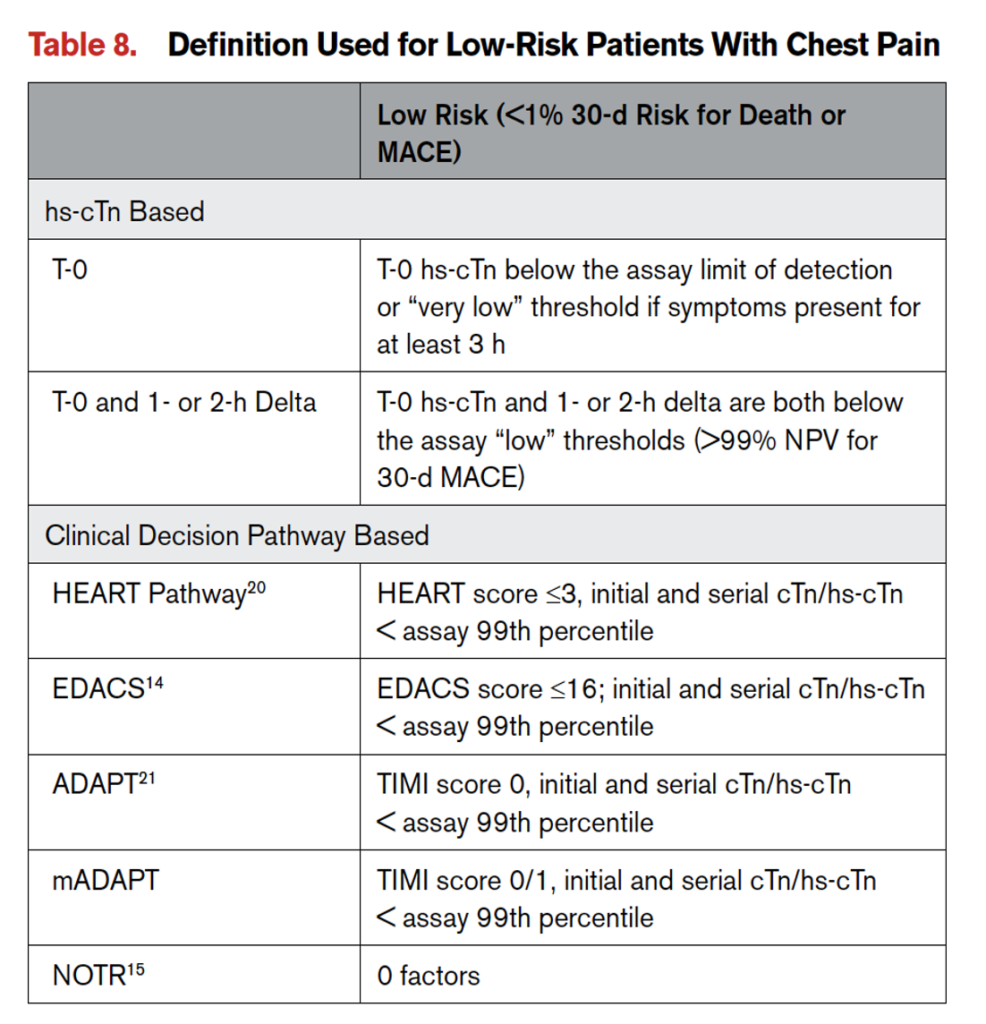
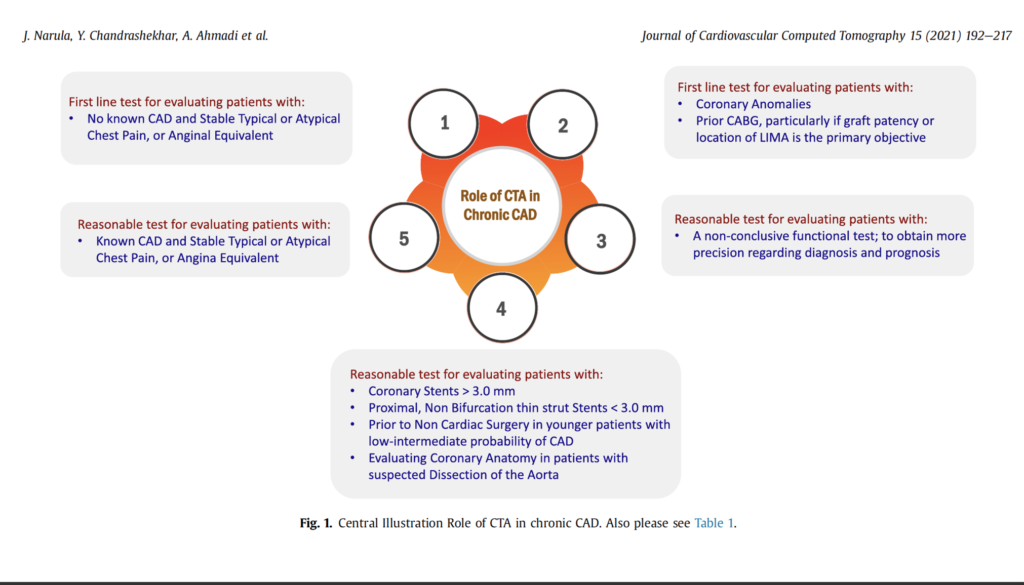
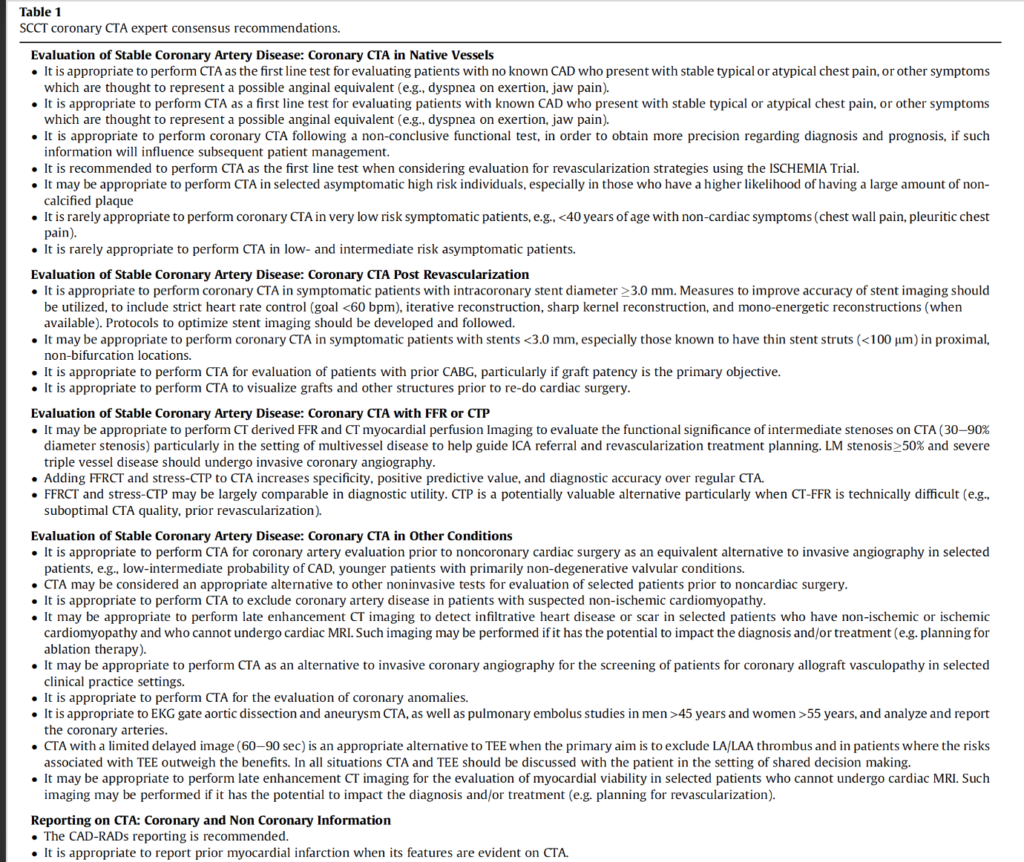
Review of Key Guidelines towards and evidence based pathway
Pathway Completion May Lead to Decreased Testing on Further Encounters if Integrated into Pathway
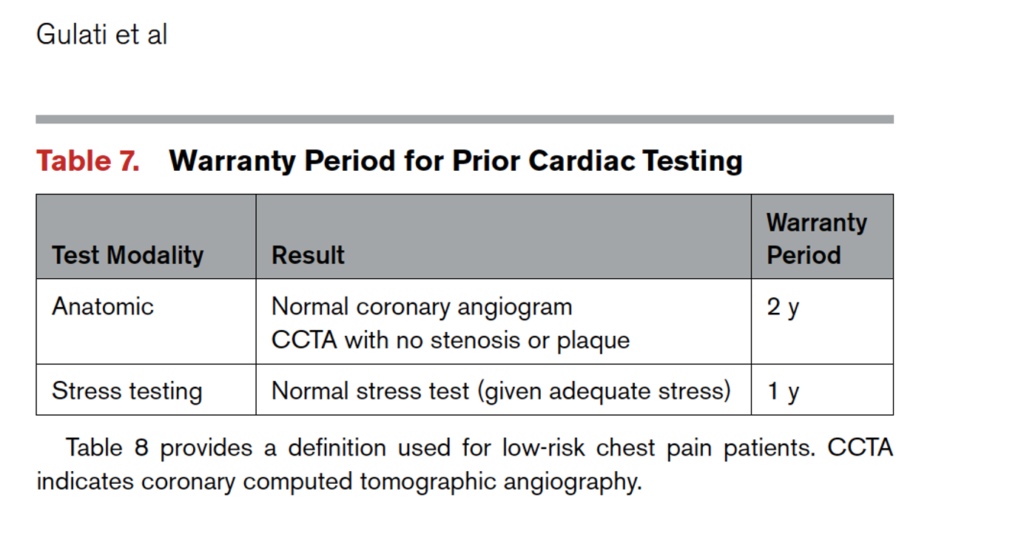
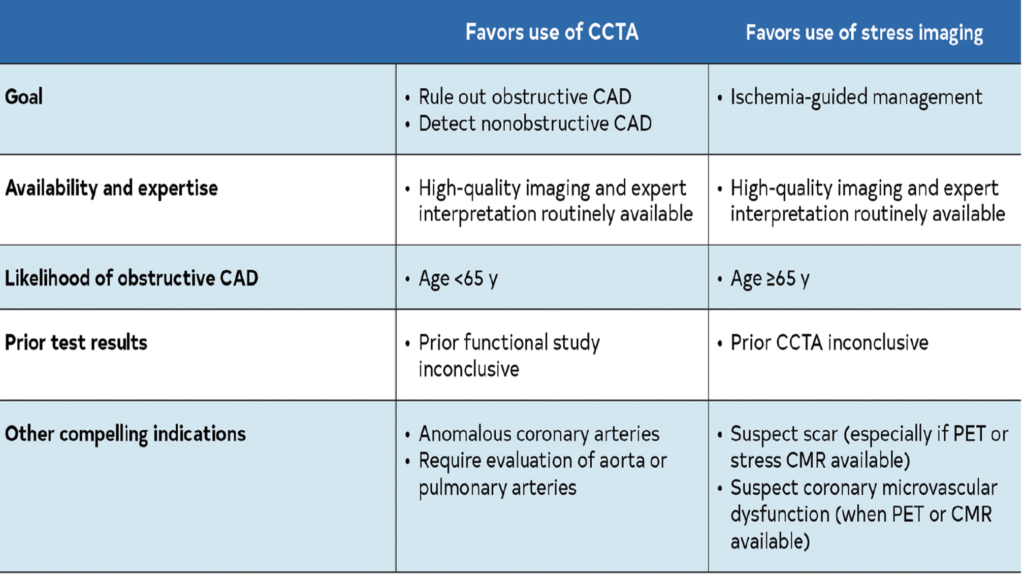
2021 Joint Consensus Guidelines Intermediate Risk Chest Pain Algorithm
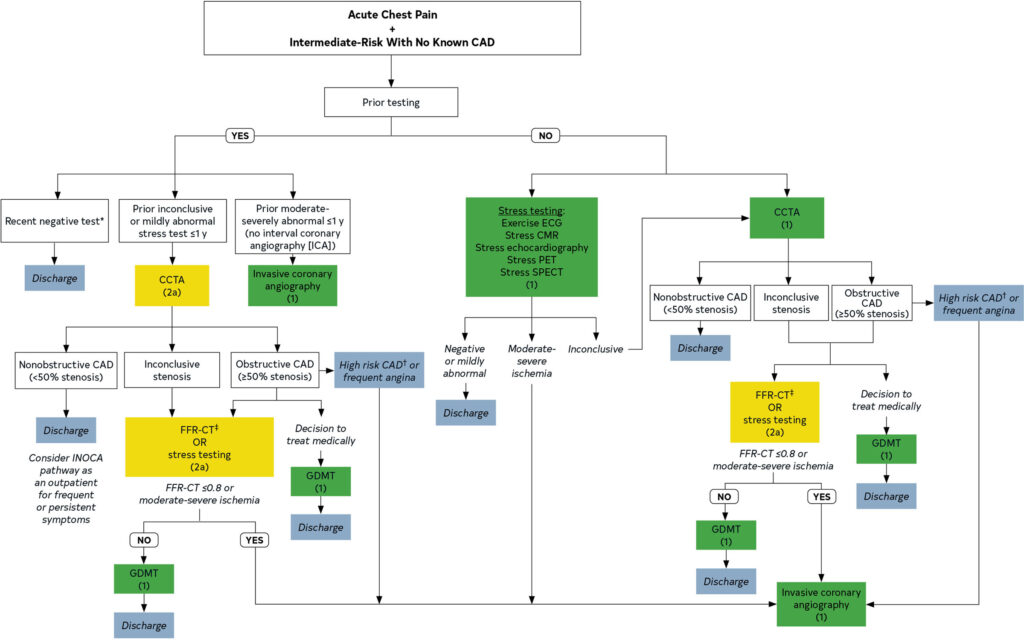
Pathway Steps and Points of Need
CCTA Leads To 7 Common Scenarios
- No Disease
- Calculate ASCVD score
- who? At ED D/C? Put all on statin who have appropriate score at D/C?)
- Routine PCP follow up (little coordination needed)
- Calculate ASCVD score
- Significant Disease > 70%
- Return to ED immediately
- Calcium Score > 133 single vessel or > 400 total
- Nuclear Stress
- Obstruction 50-70%
- In ED CDU these patients underwent cardiology c/s for decision making. A reasonable number went onto LHC.
- Obstruction < 50%
- ASCVD Score
- Coordinated PCP Follow Up
- Can not complete/can not tolerate/inconclusive/quality issue CCTA
- Nuclear Stress
- Non CAD Pathology Found on CCTA (e.g. myocardial bridge)
- Many of these patients had cardiology consult and echocardiogram
These 7 Scenarios generate coordination steps
- Transportation to CCTA
- Transportation back home from CCTA
- Payment/funding/authorization for CCTA
- Results of CCTA/Result Reporting
- Prescriptions for Statins/other medications
- PCP follow up in mild obstruction
- Cardiology Follow up in moderate or other pathology
- Nuclear Stress Testing
- Potential Transportation to return for Nuc Stress
- Telemedicine Infrastructure, Visits – pcp and cards?
Monitoring
- High risk events/dysrhythmias can occur with intermediate risk chest pain patients
- Monitoring may help identify early dysrhythmia and other deterioration
- Will we utilize monitoring in these patients at discharge?
- How will this be set up, verified, followed?
- Other issues?
Arranging Imaging/Completing Imaging
- Do we order CCTA in Epic as if it was taking place at TGH? Is there another system/way to do this for the Tower Patients?
- What do we need to build into Epic to coordinate image scheduling?
- Does registration/finance etc need to be notified to begin working on most appropriate way to fund test?
- Are there standing med orders (e.g. b-blocker) for the CCTA? Do we order?
- Ok to initiate statin as part of pathway based on ASCVD score prior to imaging?
- Other issues?
Transportation
- Who will coordinate transportation?
- Does it matter if patient is non-vertical/wheelchair dependent?
- Will this be something that TTCC does with SW/CM?
- May need 2-3 RT transports arranged
- If not using telemedicine, may need more
- Other issues?
Following Up Imaging Results and Action Steps
- Who follows up the imaging results?
- Results must be relayed to patient but also integrated into pathway for next action step
- No disease – ASCVD, no specific coordinated follow up needed. If ASCVD high, might already have Rx for Statin or will need Rx
- Significant obstruction > 70% must tell patient to return to ER immediately and may need to facilitate
- The other scenarios require more coordination
- Further transportation
- PCP
- Cardiology
- Further Testing
- Results of Further Testing
Primary Care Access
- Moderate and Minimal Disease patients will need PCP
- PCP may be involved in statin and ASCVD
- PCP may also be needed for non CAD pathology
- PCP will also be needed after clearance by cardiology or in conjunction with other discovered disease during this pathway or cardiology workup
- How will PCP f/u be arranged? Who? USF/TTCC?
- Other Issues?
Specialty Care/Cardiology Access
- Diagnostic Test Access is a significant reason for hospital obs disposition
- We have to ensure imaging access for the appropriate D/C patient
- Just as important, and difficult in the outpatient setting, is timely access to specialty care
- Hospital disposition opens up access to rapid cardiology consult
- We will need to ensure same urgency around cardiology encounter with patient actively in a virtual observation pathway
- 2-3 result scenarios from the CCTA pathway will lead to cardiology consult that would routinely be completed in the hospital before discharge
- Same issues as PCP access in terms of how/who?
- Other issues?
Secondary Testing/Downstream Testing
Pathway Enhancements/Feedback Improvements
- We will discover patients that don’t fit our categories
- Myocardial bridge and other anomalies
- Known CAD
- Multi-Visit Patients
- We will need to eventually develop clear guidelines and strategies for these scenarios
- We can’t capture every patient but we can capture 80-90%
- Patients that are more routinely observed in the hospital will be dispositioned to a pathway outside of the physical facility
- We must track outcomes and process metrics to ensure quality and also provider and system buy in
- High quality outcomes and processes should be demonstrable through data
- This data will be critical to hard wire the pathway, scale this pathway to other institutions and scale up our own pathway to other disease states
Scale Up
- There are consensus guidelines for management of chest pain
- Our ED and institution has experience implementing evidence based approaches to chest pain utilizing CCTA and observation space
- Moving this pathway into a virtual space out of the hospital follows lessons learned from Covid that high quality care can be recreated in non-traditional locations
- The infrastructure for chest pain is there but needs to be coordinated
- The algorithm might need to be refined but, overall, lends itself to identifiable decision points that can be acted upon in an out of hospital space
- Success with this pathway could open doors to other pathways for multiple disease states and a more robust observation medicine system with both physical obs and virtual obs patients