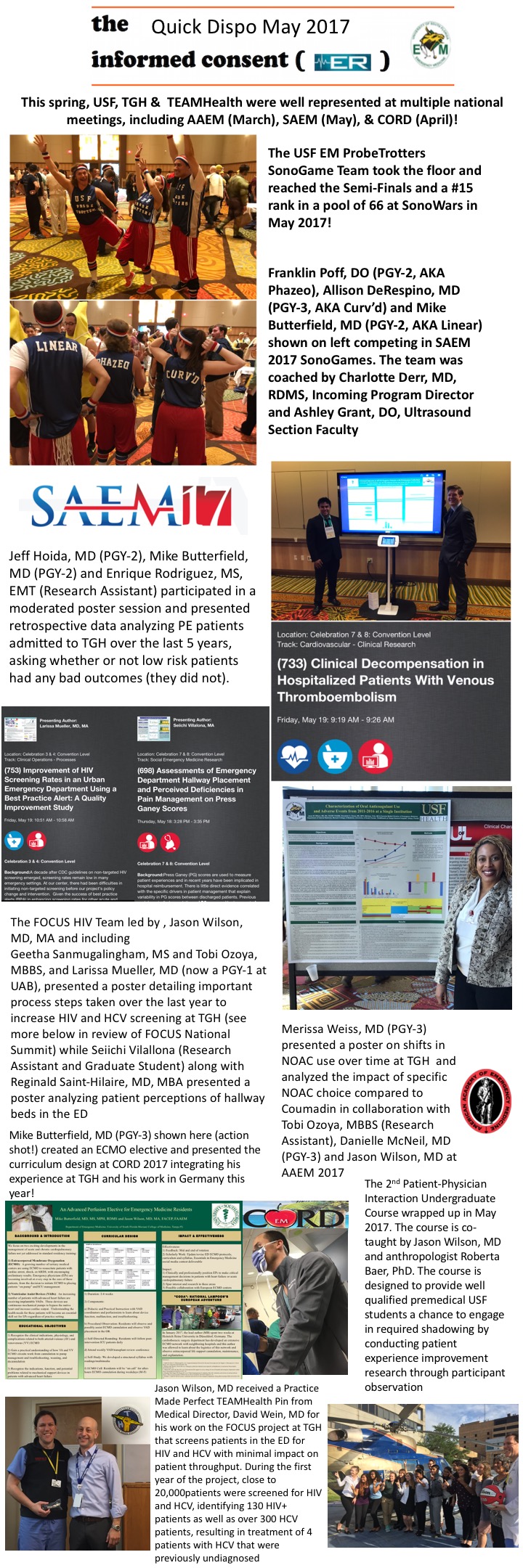
I have been guilty of under communicating in the ED – we are busy and we want to move on to the next patient. However, graduate student Seiichi Villalona and PGY-3 Christian Jeanot, MD, along with undergraduate Mery Yunez Yucosa have all been working to demonstrate the value of professional video translation services in the ED.
I have been guilty of under communicating in the ED – we are busy and we want to move on to the next patient. However, graduate student Seiichi Villalona and PGY-3 Christian Jeanot, MD, along with undergraduate Mery Yunez Yucosa have all been working to demonstrate the value of professional video translation services in the ED.
Seiichi has concentrated on showing how issues of undercommuniqation also lead to issues of healthcare autonomy and link to the important concept of healthcare deservingness.
A short but important viewpoint article from Emergency Medicine physician Breen Taira, MD, MPH appears in JAMA today echoing these themes related to undercommuniqation. Her article is at this link and below.
For what it is worth, we now have an enterprise license for the Cyracom Video Intrepreation Application for use during clinical encounters. If you want to use this service – please see the last TGH/TEAMHealth Weekly Update.
Breena R. Taira, MD, MPH, CPH
Department of Emergency Medicine, Olive View–UCLA Medical Center, Sylmar, California. ([email protected]).
It was my first day of clinical rotations as a third-year medical student. We entered a small room in the emer- gency department to see a frightened woman with acute cholecystitis. One physician asked her how she was feel- ing, but after another physician said “Spanish-speaking only,” the first physician stopped speaking and instead approached the bedside and began to push on her ab- domen. “¿Dolor? ¿Dolor?” he asked. When the patient gri- maced, the first physician, apparently satisfied with his evaluation, turned and led the team out of the room. No explanation was offered to the patient. I hesitated, hop- ing to explain, or perhaps comfort her, but this elicited a stern look. “Hurry up—the OR starts in 20 minutes!” This was my introduction to a medical culture that nor- malizes undercommunication with patients of limited English proficiency.
Undercommunication potentially affects large num- bers of patients. According to the 2011 American Com- munities Survey, more than 60 million people in the United States speak a language at home other than English, and of those, 42% report that they speak English less than “very well.”1 Although regional variation in the frequency of encounters with patients of limited English proficiency is to be expected, in cities such as Los Angeles, it is the norm, not the exception.
As a physician in a large institution, I am well aware that patients will typically encounter multiple physicians, nurses, and other staff members before I meet them. And yet, too frequently when I meet the patient, the preferred language has not yet been identified. I saw a patient referred for “continuous crying.” I was told that the patient was nonverbal, and that the plan was to ad- mit to the medicine service to “rule out acute coronary syndrome.” When I took over care, the patient had been in the emergency department all day. I noted the eth- nicity of the name and recognized that—as it hap- pened—I might know the patient’s language. So I asked in that language how the patient was feeling. To every- one’s surprise, the patient answered appropriately. When asked the reason for crying, the patient described foot pain. On examination, the patient had a large sore on the heel. All day, without an interpreter, the patient had not been able to tell anyone the source of pain or receive treatment, let alone explain what had happened. After obtaining additional history with the help of a video- based interpreter, the cardiac workup was aborted, and the patient received appropriate wound care and pain control.
This is surely an extreme case, but it demonstrates that undercommunication may be accepted as the norm when caring for patients with limited English profi- ciency. A more typical, and more insidious, scenario goes like this: a clinician who speaks a bit of Spanish tries to muddle through an interview with a Spanish-speaking patient without an interpreter. The clinician leaves the room satisfied—she has, after all, figured out that the pa- tient’s ankle, knee, and elbow have been injured, which has enabled the ordering of every one of the appropri- ate radiographic images. The fact that the injuries re- sulted from an episode of domestic violence, however, remains undiscovered, and the patient remains in dan- ger. The implications of compromised communication on health outcomes are not immediately apparent, so “muddling through” visits with patients with limited English proficiency becomes an ingrained and ac- cepted practice pattern.
Patients with limited English proficiency achieve less symptom control than those who are English proficient,2 are subject to more liberal use of testing,3 and have higher rates of unplanned revisits to the emergency depart- ment after hospital discharge.4 As a protection against in- adequate care, federal law requires language assistance for such patients. Title VI of the 1964 US Civil Rights Act bans discrimination based on race, color, or national ori- gin, which is interpreted to include those with limited English proficiency, and allows forfederal funds to be with- held if discrimination is found.5 All health care facilities that receive federal money must provide language assis- tance to patients with limited English proficiency.
Lack of knowledge and enforcement perpetuate un- dercommunication. Even when available, language as- sistance is underutilized.6 Although clinicians may agree in theory that clear communication is paramount, true 2-directional communication takes time, and clinicians may accept undercommunication as a trade-off in the name of efficiency.7 They may use their own nonfluent language skills, even while knowing that the patient might not completely understand them. Patients strain to express themselves in broken English, and clinicians use their 20-word Spanish vocabulary, while video in- terpreter machines remain unused in a back hallway. Poor communication facilitates the persistence of health disparities on a population level
Addressing undercommunication is a matter not only of social justice, but also of patient safety and qual- ity of care. Proposed solutions should focus on chang- ing the decision architecture: how to make it easier for clinicians to do the right thing. Hospital systems and medical offices should support clinicians in their use of language assistance. At registration, the patient’s pref- erence for language assistance should be identified and prominently displayed in the medical record. Language assistance should be readily available and easy to use. Each patient room should have a phone with the inter- preter line on speed dial. If internet-based video inter- preter machines are used, the health care facility should assure sufficient internet capacity to minimize wait times and dropped calls. Health care organizations should proactively moni- tor quality indicators for the care of patients with limited English pro- ficiency and improve their communications systems when deficien- cies are found.
Placing language assistance directly at the disposal of the pa- tient is a complementary approach. A language advocate can visit hospitalized patients with limited English efficiency to teach about the right to language assistance and how to dial an interpreter.9 Elimi- nating the clinician’s role in the decision to involve an interpreter can improve communication and promote patient autonomy.
Access to a clinician who speaks the same language as the pa-tient may also improve care and health outcomes.10 Standards, training, and credentialing for the use of languages other than English by clinicians, however, should be implemented to assure compe- tence, just as they are for physicians who perform invasive proce- dures. Clear and 2-directional communication with patients with lim- ited English proficiency should be the rule, not the exception.
Published Online: March 19, 2018. doi:10.1001/jamainternmed.2018.0373
Additional Contributions: I would like to acknowledge Jerome Hoffman, MD, Professor Emeritus, UCLA Department of Emergency Medicine, for his input on this article. Dr Hoffman was not compensated for his input.
REFERENCES
- Ryan C. Language Use in the United States: 2011. 2013. https://www.census.gov/prod/2013pubs/acs-22.pdf. Accessed January 24, 2018.
- Chan A, Woodruff RK. Comparison of palliative care needs of English- and non-English-speaking patients. J Palliat Care. 1999;15(1):26-30.
- Hampers LC, McNulty JE. Professional interpreters and bilingual physicians in a pediatric emergency department: effect on resource utilization. Arch Pediatr Adolesc Med. 2002;156(11): 1108-1113.
- Ngai KM, Grudzen CR, Lee R, Tong VY, Richardson LD, Fernandez A. The association between limited English proficiency and unplanned emergency department revisit within 72 hours. Ann Emerg Med. 2016;68(2):213-221.
- Equal Employment Opportunity Program. Title VI, Prohibition Against National Origin Discrimination Affecting Limited English Proficient Persons: National Archives and Records Administration. 2004. https://www.archives.gov/eeo/laws/title-vi.html. Accessed June 7, 2017.
- Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. J Health Care Poor Underserved. 2008;19(2):352-362.
- Diamond LC, Schenker Y, Curry L, Bradley EH, Fernandez A. Getting by: underuse of interpreters by resident physicians. J Gen Intern Med. 2009;24 (2):256-262.
- Karliner LS, Pérez-Stable EJ, Gregorich SE. Convenient access to professional interpreters inthe hospital decreases readmission rates and estimated hospital expenditures for patients with limited English proficiency. Med Care. 2017;55(3): 199-206.
- Basu G, Costa VP, Jain P. Clinicians’ obligations to use qualified medical interpreters when caring for patients with limited English proficiency. AMA J Ethics. 2017;19(3):245-252.
- Parker MM, Fernández A, Moffet HH, Grant RW,
Torreblanca A, Karter AJ. Association of patient-physician language concordance and
glycemic control for limited-English proficiency Latinos with type 2 diabetes. JAMA Intern Med. 2017;177(3):380-387.




 I have been guilty of under communicating in the ED – we are busy and we want to move on to the next patient. However, graduate student Seiichi Villalona and PGY-3 Christian Jeanot, MD, along with undergraduate Mery Yunez Yucosa have all been working to demonstrate the value of professional video translation services in the ED.
I have been guilty of under communicating in the ED – we are busy and we want to move on to the next patient. However, graduate student Seiichi Villalona and PGY-3 Christian Jeanot, MD, along with undergraduate Mery Yunez Yucosa have all been working to demonstrate the value of professional video translation services in the ED. Discuss patients you have seen with the undergraduate ANT4930 students this semester. This day is always a favorite for the students – even if you can only spend 15 minutes with the class, the students will get A LOT from your insight. Please help us continue making this day a success. Thanks to Rachel Semmons, Jim Gillen, Melissa Leming, Reggie Saint-Hillaire, David Wein, Tabitha Campbell and anyone I may have forgot, who have all participated in prior years.
Discuss patients you have seen with the undergraduate ANT4930 students this semester. This day is always a favorite for the students – even if you can only spend 15 minutes with the class, the students will get A LOT from your insight. Please help us continue making this day a success. Thanks to Rachel Semmons, Jim Gillen, Melissa Leming, Reggie Saint-Hillaire, David Wein, Tabitha Campbell and anyone I may have forgot, who have all participated in prior years. Also, special guest David Wein, MD, MBA will talk about medicine in New Zealand as well. Oh, and notice how he rocks the vest when he is there – maybe his vest feels threatened by my vest stateside!
Also, special guest David Wein, MD, MBA will talk about medicine in New Zealand as well. Oh, and notice how he rocks the vest when he is there – maybe his vest feels threatened by my vest stateside!